Implant dentistry has revolutionized the way clinicians restore edentulous patients, but not every case can be managed with standard implant procedures. One of the greatest challenges in implantology is dealing with patients who have insufficient bone volume in the maxilla or mandible, especially in the posterior regions. In such situations, remote anchorage provides a crucial solution.
Remote anchorage refers to the placement of implants in structures that are anatomically distant from the original edentulous site, such as the zygomatic bone, pterygoid bone, or mandibular symphysis, providing a stable foundation for implants. This technique allows for the restoration of both function and aesthetics, especially in cases where conventional implants cannot be placed due to bone resorption, anatomical constraints, or other factors.
This article highlights four clinical cases where remote anchorage is the best option for ensuring optimal implant stability and improving patient outcomes.
1. Severe Maxillary Atrophy
Maxillary atrophy is a common condition encountered in edentulous patients, especially those who have been missing teeth for an extended period. This leads to the resorption of the maxillary alveolar ridge, making traditional dental implant placement challenging. When the bone volume is insufficient, remote anchorage in the form of zygomatic implants becomes the best solution.
A. Clinical Scenario:
A 65-year-old male patient presents with a completely edentulous maxilla due to periodontal disease and years of tooth loss. Upon evaluation, the maxillary alveolar ridge shows severe resorption, especially in the posterior maxilla. CBCT imaging reveals that there is no adequate bone height or width in the posterior regions to place traditional dental implants. The patient is in good overall health and desires a permanent, functional solution to restore his dentition.
B. Why Remote Anchorage is the Best Option:
In this case, zygomatic implants offer a solution by anchoring into the zygomatic bone (cheekbone), which is a dense, stable bone structure. Zygomatic implants are longer than traditional implants and are inserted at an angle into the zygomatic bone, bypassing the need for bone grafting or sinus lift procedures.
By using remote anchorage in the zygomatic bone, this patient can achieve immediate functional and aesthetic restoration with full-arch fixed prostheses. This approach eliminates the need for extensive bone grafting, minimizes surgical risk, and allows for the immediate loading of implants, providing the patient with a faster recovery and restoration timeline.
2. Insufficient Bone Volume in the Posterior Maxilla
One of the primary reasons remote anchorage is used is to address insufficient posterior maxillary bone volume. In many edentulous patients, the bone in the posterior maxilla undergoes significant resorption due to the lack of tooth support, often accompanied by sinus expansion. This makes implant placement in the posterior maxilla challenging.
A. Clinical Scenario:
A 50-year-old female patient presents with a severely resorbed maxillary posterior ridge and an enlarged maxillary sinus. After multiple failed attempts to place conventional implants, the patient’s existing bone is too thin and low in height to support traditional implants. Sinus lift procedures were attempted but were unsuccessful, leaving the patient with no viable options for restoring her posterior teeth.
B. Why Remote Anchorage is the Best Option:
In this case, pterygoid implants are the best solution. Pterygoid implants are placed in the pterygoid bone, which lies behind the maxilla, close to the pterygoid plates of the sphenoid bone. The pterygoid region provides dense, stable bone that can anchor dental implants effectively, bypassing the need for a sinus lift.
The pterygoid implants provide the necessary stability for a full-arch restoration, offering the patient the possibility of immediate implant loading and a fixed prosthesis. This technique has a high success rate and is less invasive than other approaches, such as bone grafting, while delivering superior functional and aesthetic results.
By utilizing remote anchorage in the pterygoid region, this patient can regain functional occlusion and aesthetics with minimal surgical intervention.
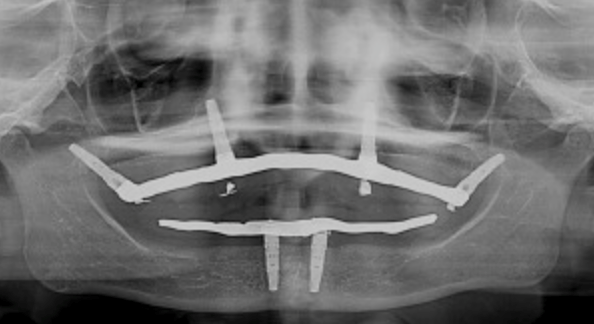
3. Mandibular Atrophy in the Posterior Region
While maxillary bone resorption is common, posterior mandibular atrophy can also create difficulties in implant placement. In such cases, mandibular symphysis implants or anterior mandibular implants can be utilized as part of a remote anchorage strategy to ensure stability and support for the restoration.
A. Clinical Scenario:
A 70-year-old male patient presents with severe posterior mandibular bone loss, resulting from years of tooth loss and subsequent resorption of the alveolar ridge. The patient desires a full-arch restoration for the lower jaw but has insufficient bone in the posterior mandible to support conventional implants. Further, his posterior ridge has become so thin that bone grafting is not a feasible option due to the risk of nerve injury.
B. Why Remote Anchorage is the Best Option:
For this patient, anterior mandibular implants, which are placed at the mandibular symphysis, offer the best solution. The mandibular symphysis is located in the midline of the mandible and typically has more available bone mass than the posterior regions. By placing implants in this area, the implant forces are better distributed, and the overall stability of the restoration is enhanced.
In some cases, transmandibular implants (which extend through the entire mandible) may also be considered for more challenging scenarios. These implants can anchor into the denser bone of the anterior mandible, providing the necessary foundation for a full-arch lower prosthesis, and can often be loaded immediately.
By using the anterior mandible or symphysis as a stable anchor point, remote anchorage ensures a stable restoration in cases where posterior mandibular bone loss would preclude traditional implant placement.
4. Severe Craniofacial Defects and Trauma Reconstruction
Patients who have experienced craniofacial trauma or congenital craniofacial defects may have significant loss of bone structure, making conventional dental implants impossible. In these cases, remote anchorage in the zygomatic bone, temporal bone, or other craniofacial regions can offer the only viable option for implant placement.
A. Clinical Scenario:
A 30-year-old male patient presents with severe facial trauma resulting from a car accident. The patient has suffered significant damage to the maxillary and zygomatic bones, leaving his anterior and posterior maxillae severely compromised. The remaining bone is insufficient to support conventional implants. The patient seeks restoration of both function and aesthetics, including the replacement of lost teeth in the maxillary arch.
B. Why Remote Anchorage is the Best Option:
In this case, zygomatic implants placed into the zygomatic bone offer the best solution. These implants bypass the damaged maxillary alveolar ridge and anchor into the robust zygomatic bone, allowing for immediate restoration of both the teeth and the surrounding soft tissues. The zygomatic bone offers excellent stability due to its dense bone structure, and implant placement here can provide the necessary support for a full-arch restoration, even in the face of severe craniofacial deformity.
Zygomatic implants not only restore function but also improve the patient’s appearance, providing a durable and aesthetic solution where conventional implant placement would be impossible. The ability to load these implants immediately further improves the patient’s rehabilitation, as they can leave with a functional restoration on the same day as surgery.
Conclusion
Remote anchorage has become an invaluable tool in the field of implant dentistry, especially for patients with severe bone loss or compromised anatomical structures. Whether through zygomatic implants, pterygoid implants, mandibular symphysis implants, or craniofacial implantology, remote anchorage offers viable alternatives when traditional implant placement is not possible.
The four cases outlined in this article demonstrate the versatility and efficacy of remote anchorage in addressing some of the most complex and challenging implant cases. By utilizing stable, distant anatomical structures for anchorage, clinicians can achieve optimal outcomes in patients who otherwise would not have viable options for implant restoration. With proper planning, advanced surgical techniques, and the right indications, remote anchorage is undoubtedly one of the best options for restoring function and aesthetics in complex implant cases.