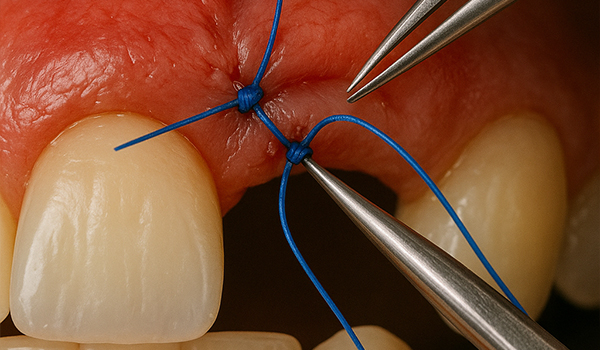
In implant surgery, achieving successful outcomes goes beyond the precise placement of the implant itself. Soft tissue management plays a crucial role in ensuring proper healing, minimizing complications, and securing long-term implant success. One of the most fundamental aspects of soft tissue management is suturing—a skill that requires both technical expertise and an understanding of the anatomy, physiology, and healing processes of the oral tissues.
As a trained dentist specializing in implantology, mastering the art of suturing is essential for optimizing surgical outcomes and promoting tissue healing. In this blog post, we will explore suturing techniques in the context of implant surgery, offering practical tips to help you refine your skills and improve patient outcomes.
Why Suturing Matters in Implantology
Proper suturing is vital in implantology for several reasons:
- Tissue Adaptation and Healing: A well-placed suture helps secure the soft tissue around the implant site, ensuring the tissue heals in the correct position. Good tissue closure promotes faster healing and reduces the risk of infection, dehiscence, or other complications.
- Minimizing Post-Operative Discomfort: Proper suturing minimizes trauma to the tissues, leading to less pain and swelling for the patient. Smooth, clean closures can significantly enhance patient comfort during the recovery period.
- Aesthetic Outcomes: Especially in the esthetic zone (e.g., anterior teeth), the way the tissue heals around the implant is critical to the final appearance. A well-executed suture can help achieve a natural-looking gum line that blends seamlessly with the implant restoration.
- Preventing Complications: Proper suturing technique reduces the risk of complications like flap dehiscence, necrosis, or post-operative infection. A clean closure ensures that the wound is properly sealed and protected during the healing phase.
Suturing Techniques for Implant Surgery
There are several suturing techniques that can be used during implant surgery, each with its own advantages depending on the situation. Let’s break down the most common suturing techniques and their applications in implantology.
1. Interrupted Sutures
Interrupted sutures are one of the most commonly used sutures in implant surgery. This technique involves placing individual knots at each suture point, allowing for precise tension control at each segment of the wound.
- Indications: Ideal for areas that need a high degree of tension, such as around implant sites where tissue closure is crucial for proper healing. It is also useful in cases where tissue thickness varies along the incision line.
- Advantages: Allows for localized adjustment of tension, providing more control over the closure and enabling excellent adaptation of the tissue.
- Technique: The suture is passed through the tissue at the edge of the incision, then pulled tight and tied off. A new suture is placed at the next point, creating individual “tacks” along the incision line.
2. Continuous Sutures (Running Sutures)
The continuous suture involves a single thread that runs along the length of the wound, with no interruption between the individual knots. This technique is faster to place than interrupted sutures and is commonly used for longer incisions.
- Indications: Useful for closing longer incisions or flap designs, such as in full-thickness flap procedures for implant placement. It is also commonly used in the posterior region where tension and aesthetic concerns are less critical.
- Advantages: Faster and easier to place than interrupted sutures, and the even distribution of tension helps to achieve a smooth, uniform closure.
- Technique: The suture is passed continuously through the tissue, with each bite pulled tightly in sequence. The thread is then tied off at the end of the incision.
3. Vertical Mattress Sutures
The vertical mattress suture is a technique that provides excellent wound closure under moderate tension. This technique passes the suture through the tissue at two levels—superficial and deep—creating a tension-free closure at the surface while securely approximating deeper tissues.
- Indications: Ideal for areas where tissue mobility is greater, such as the lower anterior mandible or areas with thicker soft tissue. This technique is particularly useful for socket preservation procedures or when suturing around large implant sites where additional tension relief is necessary.
- Advantages: The technique creates a strong, secure closure, distributing tension evenly across the wound. It also allows for the precise adaptation of both the superficial and deep layers of the tissue.
- Technique: The suture passes vertically through the tissue at both a deep and superficial level, drawing the tissue together and creating a secure closure with less tension on the surface.
4. Horizontal Mattress Sutures
Horizontal mattress sutures involve passing the suture in a horizontal direction across the incision and tying it to secure the tissue. This technique is effective at preventing tissue tension at the wound edges and is often used in cases where the tissue is thin or the incision line is under tension.
- Indications: Best for closing larger flaps or incisions with tension, particularly in areas where the tissues are thin and prone to dehiscence.
- Advantages: This technique provides a strong, broad suture grip on the tissue, which is particularly beneficial for preventing flap dehiscence in high-tension areas. It also promotes tension-free healing in the superficial layers of the tissue.
- Technique: The suture is passed horizontally through the tissue and then tied, with the knot lying above the incision line to reduce tension on the flap.
5. Tension-Free Flap Closure
In implant surgery, it’s crucial to avoid placing excessive tension on the tissue flaps, as this can compromise blood flow to the area and impair healing. The tension-free flap closure technique focuses on securing the tissue with minimal tension, which is especially important in esthetic areas and around dental implants.
- Indications: Used in delicate procedures where maintaining blood supply to the tissue is critical. For example, in anterior implant surgeries, especially in the aesthetic zone, this technique is crucial for ensuring healthy gum healing.
- Advantages: Promotes faster, more predictable healing with minimal scarring or complications.
- Technique: The goal is to trim and reposition tissue flaps so that they naturally lie in a position that doesn’t pull on the surrounding tissues. The flap is then sutured using techniques like interrupted or continuous sutures to achieve a tension-free closure.
Selecting the Right Suture Material
Choosing the right suture material is equally important as selecting the correct technique. The material you choose will depend on the tissue type, the location of the incision, and the desired outcome. Here are some common options used in implant surgery:
- Absorbable Sutures (e.g., Vicryl, Monocryl): These sutures are designed to dissolve over time, eliminating the need for removal. They are ideal for deep tissue sutures or for areas where post-operative visits might be difficult.
- Non-Absorbable Sutures (e.g., Nylon, Prolene): These sutures do not dissolve and require removal after healing. They are typically used for superficial sutures in areas that require greater strength or where the wound will be under tension.
- Monofilament vs. Braided Sutures: Monofilament sutures (e.g., Prolene) have a single, smooth strand and are less likely to harbor bacteria, reducing the risk of infection. Braided sutures (e.g., Vicryl) are stronger but may increase the risk of infection due to their structure.
Tips for Successful Suturing in Implant Surgery
- Tissue Handling: Always handle tissues gently and avoid crushing or tearing them. Use sharp instruments to minimize trauma and preserve the blood supply.
- Suture Tension: Ensure that sutures are not placed too tightly, as excessive tension can compromise circulation and delay healing. The tissue should be snugly adapted, but not under undue strain.
- Aesthetic Considerations: In the esthetic zone, take extra care to ensure that sutures are placed symmetrically, with the goal of achieving an ideal tissue contour. Consider using cosmetic suturing techniques, such as single, non-penetrating sutures in highly visible areas.
- Post-Operative Care: After suturing, ensure proper post-operative care instructions for your patients, including recommendations for oral hygiene, diet, and follow-up visits to monitor healing.
Conclusion: Perfecting the Art of Suturing
The ability to suture effectively is an essential skill in implant surgery that requires both knowledge and experience. By mastering techniques such as interrupted sutures, vertical and horizontal mattress sutures, and tension-free closures, you can significantly enhance the quality of your implant surgeries, promote faster healing, and improve patient outcomes.
As a trained dentist, your goal should be to combine precise surgical techniques with thoughtful soft tissue management. Through practice, education, and continuous refinement of your suturing skills, you can elevate your implantology practice and offer patients the best chance for successful, long-lasting results.