Introduction
Bone grafting has become a critical component of dental implantology, especially as the demand for implants increases among patients with compromised bone structures. Successful dental implant placement depends not only on the surgical precision of implant insertion but also on the ability to restore and maintain adequate bone volume and quality. In situations where the alveolar ridge is deficient in bone, bone grafting procedures are often employed to create a stable foundation for dental implants.
In this article, we will explore the essential aspects of bone grafting for dental implant success. This includes understanding the types of bone grafts, indications for grafting, the various techniques, and the importance of proper patient selection and post-operative care. As trained professionals, having a comprehensive grasp of these concepts is crucial for ensuring optimal outcomes in dental implant procedures.
1. The Role of Bone Grafting in Implantology
Bone grafting plays a pivotal role in preparing the implant site for the successful integration of dental implants. When patients present with inadequate bone volume or density, the risk of implant failure increases due to insufficient osseointegration. Inadequate bone can be caused by several factors, including:
- Bone Resorption: This occurs naturally after tooth extraction, particularly in the upper jaw or in the posterior regions of the mandible, where bone loss is more pronounced.
- Congenital Defects: Some patients may have an inherently small or malformed alveolar ridge due to genetics or developmental issues.
- Trauma: Accidents or injury to the mouth may cause bone loss, which compromises the ability to place implants.
- Periodontal Disease: Chronic infection or inflammation of the gums can result in bone loss around teeth, complicating implant placement.
Bone grafting restores bone to a site where it is insufficient or absent, allowing for the placement of implants that can support functional and esthetic restorations.
2. Types of Bone Grafts
There are several types of bone grafting materials that can be used in dental implant procedures. Each type has distinct properties, and the choice of graft material depends on the specific needs of the patient and the clinical situation.
1. Autografts (Autologous Grafts)
- Definition: Autografts are bone grafts taken from the patient’s own body, usually from areas like the iliac crest, tibia, or the mandibular symphysis.
- Advantages: Considered the gold standard due to their osteogenic potential (contain live bone-forming cells), leading to predictable healing and regeneration.
- Limitations: Require a second surgical site, increasing patient morbidity and surgical time.
2. Allografts (Allogenic Grafts)
- Definition: Harvested from human cadavers, processed and sterilized to remove immunogenic components.
- Advantages: No second surgical site needed, widely available, good osteoconductive properties.
- Limitations: Lack osteogenic cells; slower integration compared to autografts.
3. Xenografts (Xenogenic Grafts)
- Definition: Derived from animals, commonly bovine or porcine sources, and processed to remove immune-reactive proteins.
- Advantages: Readily available, cost-effective, suitable for ridge preservation and sinus lifts.
- Limitations: Not osteogenic; some patients may object to animal-derived materials.
4. Alloplasts (Synthetic Bone Grafts)
- Definition: Manufactured from synthetic materials like calcium phosphate or hydroxyapatite, mimicking the mineral structure of bone.
- Advantages: Fully synthetic (no risk of disease transmission), customizable in composition.
- Limitations: No biological activity; rely entirely on the host environment for integration.
3. Bone Grafting Techniques
Several techniques are available, and the appropriate method depends on the clinical presentation and intended outcome:
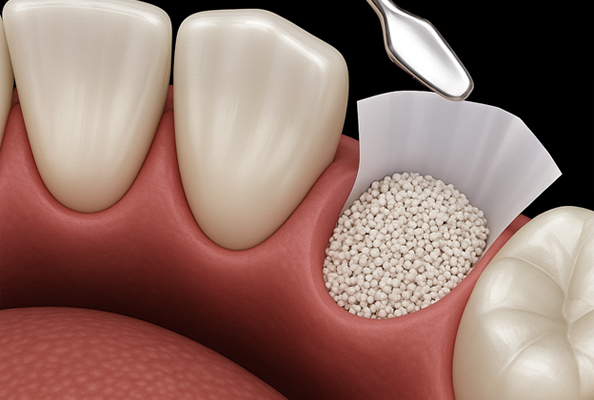
Socket Preservation (Ridge Preservation)
- Indication: After extraction to minimize resorption and preserve bone architecture.
- Procedure: Graft material is placed in the socket, sometimes with a membrane. Prevents collapse of the ridge and maintains volume.
Sinus Lift (Sinus Augmentation)
- Indication: When the posterior maxilla has insufficient height for implants due to sinus pneumatization.
- Procedure: The sinus membrane is elevated, and bone graft is placed beneath it. May be simultaneous with or prior to implant placement.
Ridge Augmentation (Horizontal and Vertical)
- Indication: Severe bone loss in ridge width or height.
- Procedure: Bone is added to the deficient area with or without barrier membranes to promote regeneration.
Block Bone Grafting
- Indication: Significant structural defects, often in esthetic zones.
- Procedure: A solid block of bone (typically autogenous) is fixed to the recipient site, allowing integration and remodeling before implants are placed.
4. Considerations for Success in Bone Grafting
Achieving successful grafting outcomes requires attention to multiple factors:
Patient Selection
- Evaluate general health, systemic conditions (e.g., diabetes, smoking), and local site conditions (e.g., infection).
- Healing potential varies, and realistic expectations must be discussed with patients.
Material Selection
- Match material to clinical need: autografts for high regenerative potential, allografts and xenografts for volume and convenience, alloplasts for biocompatibility.
Surgical Precision
- Proper technique minimizes trauma, ensures stability, and prevents complications.
- Membranes may improve success by guiding bone growth and excluding soft tissue infiltration.
Postoperative Care
- Essential for graft survival: includes antibiotics, pain management, diet instructions, and follow-up.
- Patients must avoid disrupting the graft site, particularly during early healing.
5. Potential Complications in Bone Grafting
Despite careful planning, complications may arise:
- Infection: A risk if aseptic technique or postoperative hygiene is inadequate.
- Graft Failure: May result from movement, poor vascularization, or infection.
- Neurological Injury: Particularly with mandibular grafting; attention to anatomical landmarks is critical.
- Soft Tissue Dehiscence: Can expose graft material, compromising healing.
Prompt recognition and management are essential to avoid jeopardizing implant outcomes.
Conclusion
Bone grafting is a cornerstone of modern implant dentistry, offering a reliable solution for rebuilding deficient alveolar ridges and enabling the placement of stable, functional, and esthetic implants. As implant demand grows, clinicians must remain adept in the principles and practices of bone grafting. By understanding the indications, materials, techniques, and critical success factors, dental professionals can enhance patient outcomes and build long-term success in implantology.