In dental surgery, flap techniques play a crucial role in achieving optimal aesthetic and functional outcomes, especially in periodontal and implant procedures. Whether you’re performing soft tissue grafting, periodontal surgery, or implant placement, the ability to raise and reposition a flap with precision can make all the difference in the healing process, aesthetic result, and long-term functionality.
As trained dentists, it’s important to understand the nuances of various flap techniques, how to adapt them to the specific needs of each patient, and how to balance the clinical goals of aesthetics with the functional considerations of the tissue and bone.
In this blog, we’ll explore the essential flap techniques used in dental surgery, offering tips on how to balance aesthetic and functional outcomes for the best possible results.
1. Understanding the Basics: What is a Flap in Dental Surgery?
A flap in dental surgery refers to a section of tissue that is surgically lifted from the underlying bone to gain access to a particular area of interest—whether it’s for an implant site, periodontal treatment, or soft tissue grafting. The tissue is then either repositioned or left in place to heal, and it is secured using sutures.
There are two main goals when performing flap surgery:
- Functional: To access and treat the underlying structures such as bone, root surfaces, or implants.
- Aesthetic: To ensure the tissue heals in a way that is pleasing to the eye, preserving or enhancing the smile’s natural contours.
When planning flap surgery, you must take into consideration both of these factors. A flap that’s raised too aggressively or inappropriately can compromise both function (e.g., improper implant placement or poor healing) and aesthetics (e.g., tissue recession, scarring).
2. Choosing the Right Flap Technique for the Situation
The choice of flap technique depends on the specific clinical scenario, the location of the surgery, and the desired healing outcomes. Here are some common flap designs used in modern dental surgery:
- Full-Thickness Flap:
- Also known as a “mucoperiosteal flap,” this technique involves lifting the entire thickness of the soft tissue, including both the mucosa and periosteum. It provides the most direct access to the underlying bone and is often used in periodontal surgery, implant placement, and bone grafting.
- Key benefit:
- Provides excellent visibility and access to the bone and tooth structures, making it ideal for surgical procedures that require manipulation of bone or implants.
- Aesthetic consideration:
- A well-planned full-thickness flap allows for proper repositioning of tissue and helps minimize tissue loss or unnecessary recession after healing. Careful suturing and tension-free closure are key to maintaining aesthetic harmony.
- Partial-Thickness Flap:
- This technique involves lifting only the mucosal layer, leaving the periosteum intact. It is typically used in less invasive procedures where minimal disruption to the underlying tissues is desired, such as in crown-lengthening or soft tissue grafting.
- Key benefit:
- Less trauma to the underlying bone and tissues. This approach is often preferred when preserving gingival architecture is critical.
- Aesthetic consideration:
- By preserving the periosteum, this technique helps in maintaining blood flow to the tissues, which can promote better healing with less swelling or recession.
- Envelope Flap:
- A simple flap design that involves making an incision along the gingival margin and lifting the tissue in a way that it can be repositioned without creating any vertical release incisions.
- Key benefit:
- Simple and effective, ideal for less invasive procedures where the surgeon only needs access to a limited area of the soft tissue.
- Aesthetic consideration:
- Because there are no vertical incisions, the envelope flap is less likely to cause visible scarring or recession. It is often used in aesthetic zones where tissue preservation is paramount.
- Pedicle Flap:
- A pedicle flap is raised from an adjacent site of healthy tissue, leaving one side of the flap still attached to the tissue. This is typically used in cases of tissue grafting, such as for recession coverage in periodontal surgery.
- Key benefit:
- Offers an excellent blood supply and the potential for more tissue volume, which is critical when grafting or covering exposed root surfaces.
- Aesthetic consideration:
- By utilizing tissue from a healthy adjacent site, this technique allows for more predictable and natural-looking results in grafting, especially when covering exposed root surfaces.
3. Balancing Aesthetic Goals with Functional Necessities
When performing flap surgery, there is often a tension between aesthetic outcomes and functional considerations. It’s essential to strike a balance between these two objectives to ensure both short-term and long-term success for the patient.
Here are some tips for achieving the right balance:
- Minimize Tissue Trauma:
- Careful handling of the tissue during flap elevation can help maintain the integrity of the soft tissues, preventing unnecessary damage that could result in scarring or prolonged healing time. Minimizing trauma to the tissue ensures that the aesthetic result is preserved while still gaining the access needed for the procedure.
- Proper Positioning of the Flap:
- After the surgical procedure, the flap should be repositioned in a way that promotes optimal healing and preserves the natural contour of the gingiva. Tension-free closure is critical for preventing tissue shrinkage, recession, or scarring. Take care to ensure the tissue margins are well-approximated for proper healing.
- Avoid Excessive Flap Elevation:
- When raising a flap, excessive elevation or overly aggressive detachment of tissue can compromise both functional and aesthetic outcomes. By elevating only as much as necessary for the procedure, you can help reduce the risk of tissue necrosis, recession, or esthetic compromise post-surgery.
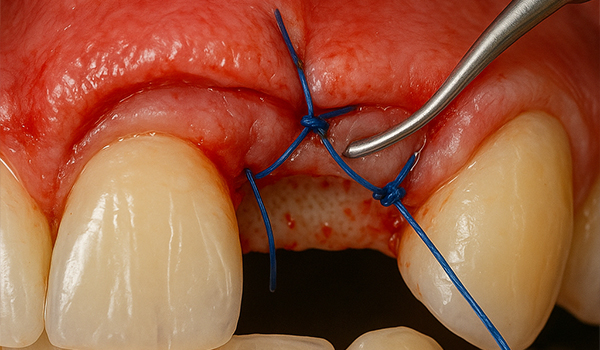
- Suture Techniques and Tension-Free Closure:
- Proper suturing is essential for both functional and aesthetic results. A tension-free suture technique allows the tissues to heal without restriction, reducing the risk of gingival recession or scar formation. Pay close attention to the placement of sutures around the flap’s margins to ensure that the tissue is securely closed without compromising blood flow.
- Consider the Aesthetic Zone:
- When performing procedures in the anterior (aesthetic) zone, special care must be taken to avoid visible scarring or tissue displacement. Techniques such as the envelope flap or using gingival displacement rather than incisions through the aesthetic zone can help preserve the appearance of the soft tissue.
Case Study: Balancing Aesthetics and Function in Periodontal Surgery
A patient with severe recession in the anterior maxillary region required periodontal surgery to address both the functional (root coverage) and aesthetic (gum contour) concerns. We used a pedicle flap technique to gain access to the underlying tissue while preserving the integrity of the adjacent healthy tissue. The flap was repositioned in a tension-free manner, and healing was monitored closely. The result was a natural-looking contour with complete root coverage and improved gingival architecture that harmonized with the patient’s smile.
Key Takeaway:
For procedures in the aesthetic zone, it’s essential to minimize tissue trauma, carefully plan flap elevation and repositioning, and ensure that sutures are placed with the utmost care to avoid scarring and ensure a natural, aesthetically pleasing result.
4. Post-Surgical Care: Supporting Aesthetic and Functional Healing
The success of any flap technique depends not only on the surgical execution but also on the post-operative care that follows. Proper healing is essential for both functional recovery and aesthetic restoration. Here are a few important post-surgical tips:
- Maintain a Clean and Stable Surgical Site:
- Ensure the patient follows oral hygiene instructions to prevent infection, but advise them to avoid disturbing the surgical site directly for the first few days.
- Monitor for Complications:
- Regular follow-up visits are crucial to monitor for potential complications such as infection, flap necrosis, or delayed healing. Early intervention can address issues before they affect both aesthetic and functional outcomes.
- Manage Swelling and Discomfort:
- Prescribe appropriate pain relief and anti-inflammatory medications to reduce swelling and ensure patient comfort during the healing period.
Key Takeaway:
Effective post-operative care is vital for ensuring the flap heals in a functional and aesthetic manner. Preventing complications through careful monitoring and providing clear instructions to patients can help achieve the desired outcome.
Conclusion: Mastering Flap Techniques for Optimal Results
Flap techniques are an essential skill for any trained dentist, and mastering them is crucial for achieving both functional and aesthetic success in dental surgeries. By selecting the right flap design, minimizing tissue trauma, and balancing functional needs with aesthetic goals, you can significantly enhance patient outcomes, especially in sensitive areas like the anterior teeth or implant sites.
Whether you’re performing periodontal surgery, soft tissue grafting, or implant placement, understanding the balance between aesthetics and function ensures a higher rate of healing, fewer complications, and satisfied patients who leave your practice with both improved function and a natural-looking result.