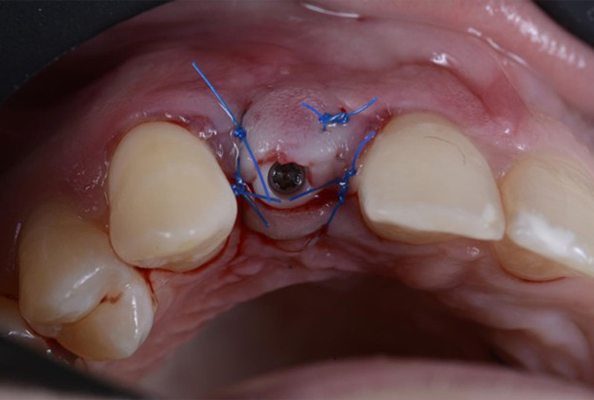
Flap design is one of the most critical aspects of implant surgery, as it directly affects the visibility, accessibility, and preservation of tissue during the procedure. Proper flap design can significantly influence the success of the surgery and the long-term stability of the dental implant. An optimized flap design enhances the surgeon’s ability to place the implant accurately, minimize complications, and promote optimal healing post-surgery.
For trained dentists, understanding the principles of flap design and adapting them to specific clinical situations is essential for achieving predictable and successful implant outcomes. This article explores the fundamentals of flap design, the various techniques used, and best practices for optimizing flap design in implant surgeries.
1. The Importance of Flap Design in Implant Surgery
The flap refers to a portion of tissue (mucosal and periosteal) that is surgically separated from the underlying bone during implant placement. Flap design serves multiple purposes:
- Visibility and Access: Provides adequate exposure to the surgical site for precise implant placement.
- Tissue Preservation: Maintains vascular integrity and protects anatomical structures.
- Postoperative Healing: Supports tension-free closure and reduces the risk of infection or wound dehiscence.
- Minimized Bone Resorption: Reduces trauma to bone surfaces, helping preserve volume and integrity.
The right flap design ensures a balance between surgical accessibility and biological preservation, contributing to long-term implant success.
2. Types of Flaps in Implant Surgery
Flap designs fall into two main categories:
A. Full-Thickness Flaps (Mucoperiosteal Flaps)
Involve elevation of both mucosa and periosteum, exposing the bone.
- Indications:
- Bone augmentation, ridge expansion, sinus lifts.
- Multiple or complex implant placements.
- Bone augmentation, ridge expansion, sinus lifts.
- Advantages:
- Excellent visibility and access.
- Allows simultaneous bone and soft tissue manipulation.
- Excellent visibility and access.
- Considerations:
- May increase postoperative swelling.
- Disrupts periosteal blood supply.
- May increase postoperative swelling.
B. Partial-Thickness Flaps (Split-Thickness)
Involve elevation of the mucosa while preserving the periosteum.
- Indications:
- Esthetic zone implants.
- Immediate implant placements.
- Esthetic zone implants.
- Advantages:
- Preserves blood supply and reduces trauma.
- Promotes faster soft tissue healing.
- Preserves blood supply and reduces trauma.
- Considerations:
- Limited surgical access.
- Technically more demanding.
- Limited surgical access.
3. Flap Design Considerations for Optimal Surgical Outcomes
Tailoring flap design to the individual case is essential. Key considerations include:
A. Access and Visibility
Ensure enough access for accurate placement, especially in complex grafting cases. Triangular or trapezoidal flaps are commonly used for posterior areas to balance access and tissue preservation.
B. Tissue Preservation and Blood Supply
Avoid excessive tension and maintain soft tissue and periosteal integrity, especially in esthetic zones where vascularity is crucial.
C. Tension-Free Closure
Always aim for a closure without tension to prevent dehiscence, promote healing, and reduce scarring. This may involve flap advancement or release techniques.
D. Aesthetic Considerations
In visible areas like the anterior maxilla, flap design must support gingival architecture and natural contours post-implantation.
4. Key Surgical Techniques for Flap Optimization
Several adjunct techniques enhance flap outcomes:
A. Flap Release
Strategically placed relieving incisions help avoid tension during closure. Careful planning protects blood vessels and nerves.
B. Mucogingival Junction (MGJ) Preservation
Preserving the MGJ supports gingival health and esthetics, particularly important in single-tooth implants in the anterior region.
C. Soft Tissue Manipulation
In cases with inadequate keratinized tissue, flap advancement, pedicle grafts, or soft tissue grafting may be needed for better healing and esthetic outcomes.
5. Conclusion
Optimizing flap design is essential for the success of dental implant surgery. A well-planned and executed flap provides the surgeon with visibility and control, preserves vital structures, ensures tension-free closure, and promotes ideal esthetic and functional results.
By understanding the principles of flap management and selecting the appropriate technique for each clinical case, clinicians can minimize complications, enhance soft and hard tissue healing, and significantly improve long-term implant outcomes. Whether performing simple placements or complex reconstructions, mastering flap design is a foundational skill for every implantologist.