In implant dentistry, the design and technique of the surgical flap play a critical role in achieving predictable, successful outcomes. The decision of which flap technique to use depends on multiple factors, including the implant site, bone quality, soft tissue condition, aesthetic concerns, and the complexity of the surgical procedure. A well-designed flap allows optimal exposure of the bone, while preserving the surrounding tissue, promoting healing, and ensuring long-term implant stability.
For trained dentists, understanding the appropriate indications for different flap techniques and how to implement them correctly is essential for maximizing surgical success and minimizing complications. This article explores various flap techniques commonly used in implant dentistry, providing guidance on when and how to use them based on clinical requirements.
1. Flap Design Considerations in Implant Surgery
Before discussing specific flap techniques, it’s important to consider the general principles behind flap design:
- Access to the Bone: The flap must provide adequate visibility and access to the implant site to facilitate precise implant placement.
- Tissue Preservation: Preserving the blood supply and minimizing trauma to surrounding tissues is crucial for proper healing.
- Aesthetic Concerns: For implants in the esthetic zone, the flap should preserve the natural contours of the gingiva to avoid post-surgical complications such as recession.
- Tension-Free Closure: The flap should be designed to ensure that when sutured, there is no tension, which could lead to delayed healing, wound dehiscence, or scarring.
The following sections discuss specific flap techniques, the indications for their use, and the clinical situations where they are most beneficial.
2. Full-Thickness Flap (Mucoperiosteal Flap)
The full-thickness flap, also known as the mucoperiosteal flap, involves the elevation of both the mucosal and periosteal layers from the underlying bone. This technique provides maximum access to the bone and is particularly useful in situations where bone grafting, complex implant placement, or significant manipulation of the bone is required.
Indications for Full-Thickness Flap:
- Bone Grafting Procedures: When extensive bone augmentation or grafting is necessary, such as in vertical or horizontal ridge augmentation, a full-thickness flap provides the best access to the bone and allows for easy placement and manipulation of bone grafts.
- Sinus Lift Procedures: A full-thickness flap is required for procedures such as sinus floor elevation, where access to the maxillary sinus and underlying bone is needed to perform the sinus lift safely.
- Multiple Implant Placements: When placing multiple implants in a single surgical session, a full-thickness flap allows for easier manipulation of the soft tissues to provide optimal access to multiple sites.
- Large Defects or Complex Sites: Full-thickness flaps are ideal for patients with extensive bone defects or in cases where anatomical landmarks (such as the inferior alveolar nerve or sinus) must be carefully navigated.
Advantages:
- Provides complete exposure of the bone, facilitating precise implant placement.
- Allows for simultaneous bone grafting and implant placement if needed.
- Suitable for complex cases requiring detailed bone preparation.
Disadvantages:
- Higher risk of postoperative swelling and discomfort due to the extensive manipulation of soft tissues.
- Potential for greater trauma to the periosteum, which can affect the vascularity of the bone and surrounding tissues.
- Increased risk of wound dehiscence and complications if flap closure is not performed properly.
Clinical Example:
In a posterior mandibular case where a sinus lift and bone grafting are needed along with implant placement, a full-thickness flap is used to access the sinus floor and ensure adequate visibility of the bone.
3. Partial-Thickness Flap
The partial-thickness flap technique involves reflecting only the mucosal layer, leaving the periosteum intact. This flap design preserves the underlying bone’s blood supply and is particularly useful in situations where minimizing trauma to soft tissues is a priority.
Indications for Partial-Thickness Flap:
- Immediate Implant Placement: After tooth extraction, the partial-thickness flap is useful when placing an implant immediately. It allows for the preservation of the vascular supply to the bone while minimizing damage to the surrounding soft tissues.
- Aesthetic Zone Implants: In the anterior maxilla or esthetic zone, preserving the soft tissue’s natural contour is essential. A partial-thickness flap minimizes damage to the soft tissues, preserving their natural architecture and blood supply.
- Less Complex Surgeries: For less complicated implant placements, where there is minimal bone manipulation and bone grafting is not required, the partial-thickness flap provides sufficient access to the implant site while maintaining the integrity of the surrounding tissues.
- Patients with Thin Gingival Biotype: In patients with a thin gingival biotype, a partial-thickness flap is often preferred to reduce the risk of gingival recession and maintain soft tissue stability post-surgery.
Advantages:
- Preserves the underlying periosteum, ensuring better blood circulation to the bone.
- Minimizes postoperative discomfort and swelling.
- Offers better soft tissue preservation, which is essential for aesthetic outcomes, particularly in the anterior region.
- Quicker healing time due to less trauma to the soft tissues.
Disadvantages:
- Limited visibility of the bone may make complex procedures like bone grafting or sinus lifts more challenging.
- May not be suitable for cases requiring significant bone manipulation or when a large area of bone needs to be exposed.
Clinical Example:
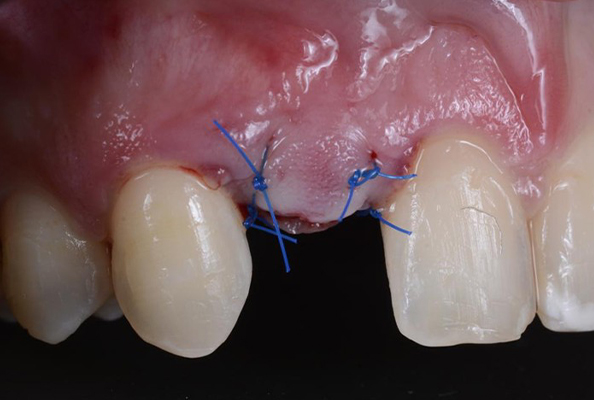
For anterior maxillary implants where aesthetic considerations are paramount, a partial-thickness flap preserves the papillary architecture and ensures minimal disruption to the surrounding gingival tissues, reducing the risk of postoperative recession.
4. Envelope Flap
The envelope flap is a flap technique that involves making an incision around the implant site, but it does not require any vertical incisions for reflection. This technique is often used in situations where only limited access to the implant site is required, and soft tissue manipulation is minimal.
Indications for Envelope Flap:
- Single Implant Placement: In cases where only one implant is being placed, particularly in the esthetic zone, the envelope flap provides enough access to the bone while minimizing trauma to surrounding tissues.
- Minimal Bone Reshaping: When the bone is already in an ideal position and only minor adjustments are necessary, the envelope flap allows for efficient implant placement with minimal disturbance to the soft tissue.
- Implants in the Mandibular Incisors or Premolars: The envelope flap is ideal for implants in these areas, where access to the bone is needed, but the flap design must minimize aesthetic complications.
Advantages:
- Minimal trauma to the soft tissues, particularly the gingiva.
- Less invasive and quicker recovery than full-thickness flaps.
- Simple to perform and suitable for cases requiring limited access.
Disadvantages:
- Limited exposure and access to the bone, which can be a drawback in more complex cases.
- Not suitable for situations requiring significant bone grafting or manipulation.
Clinical Example:
For a single implant in the mandibular incisor region, where only minimal bone reshaping is needed, the envelope flap technique is ideal for quick and efficient implant placement with minimal impact on the gingival architecture.
5. Sulcular or Crestal Flap
The sulcular or crestal flap involves making an incision along the sulcus or crestal line of the alveolar ridge, typically used for implants in areas where there is minimal bone loss and where preserving the gingival margin is important.
Indications for Sulcular or Crestal Flap:
- Immediate Implant Placement: This flap is commonly used for immediate implants, where the flap is designed to preserve the natural gingival margins after tooth extraction.
- Minimally Invasive Cases: For implants placed in areas where bone resorption is minimal, and soft tissue preservation is a priority, the crestal flap allows access without extensive tissue manipulation.
Advantages:
- Preserves the gingival architecture, which is important for esthetics, especially in the anterior region.
- Quicker recovery and less postoperative discomfort.
- Ideal for single-tooth implants and esthetic zone procedures.
Disadvantages:
- Limited visibility and access to the bone, making it less suitable for complex cases that require extensive bone manipulation.
Clinical Example:
For a single-tooth implant in the anterior maxilla, a crestal flap preserves the natural gingival margin and minimizes the risk of esthetic complications such as gingival recession.
6. Conclusion
Flap design plays a critical role in the success of implant surgeries. Choosing the right flap technique depends on multiple factors, including the complexity of the procedure, the need for bone grafting, the location of the implant, and the aesthetic demands of the patient. By understanding the indications and advantages of each flap technique—whether it’s a full-thickness flap, partial-thickness flap, envelope flap, or sulcular flap—trained dentists can optimize their approach to implant surgeries, ensuring better outcomes and minimizing complications. With proper flap management, it is possible to achieve a balance between efficient surgical